Every year the Association of American Medical Colleges (AAMC) compiles a survey of intern, resident, and fellow salaries across the country. While most medical and surgical residents are paid similar stipends, there are certainly differences. This will become a somewhat important factor in ranking residency programs during the fourth year of medical school. The recent AAMC resident and fellow stipend report can be found here as a pdf document. The complete document describes current resident salaries and displays a chart of the average resident salaries all the way back to the 1960s. Additionally, it details the difference in stipends between the northeast, the south, the west, and the midwest. Finally, it explains in detail what is included in the average benefits packages (i.e. medical insurance premiums, retirment plans, life insurance, disability ect).
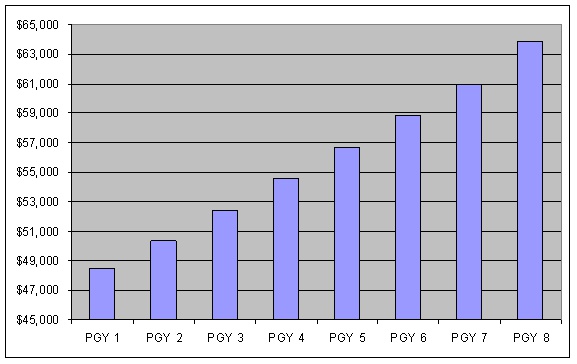
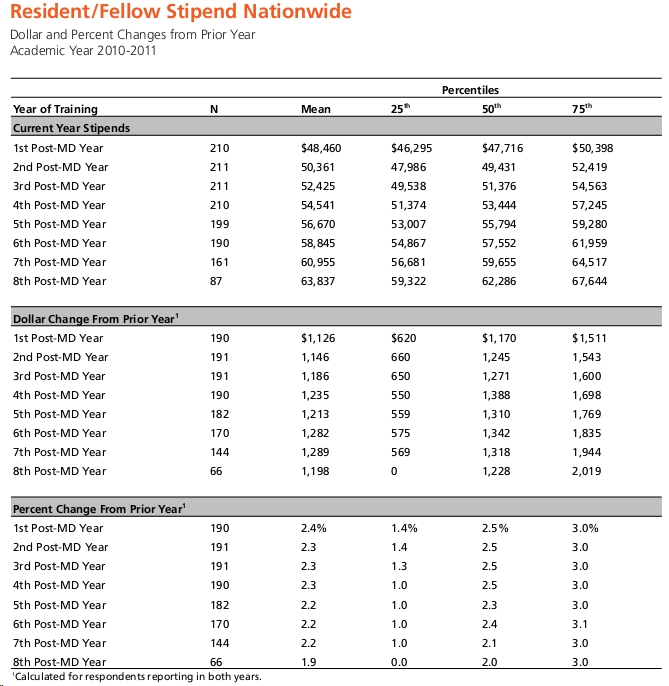
The report contains salary information for all training levels, intern thru post graduate year (PGY) eight. The national mean salary of each PGY level and the percent change from 2010 is shown below. (taken from the AAMC document)
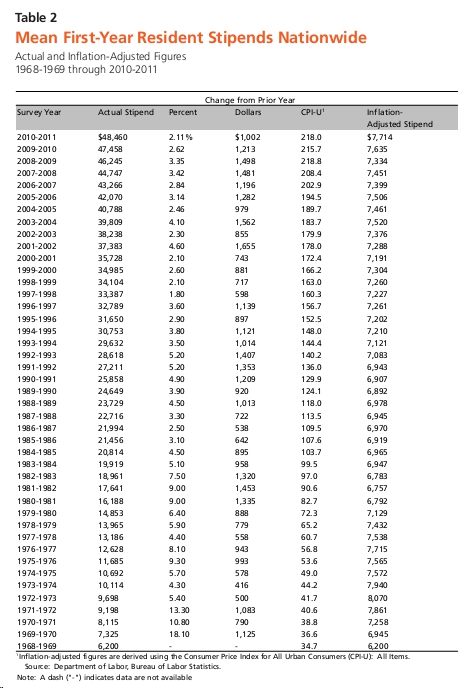
The next table displays the average first year resident (i.e. ‘intern’) salary each year since 1968. The average increase in salary in recent years has been 2-4%.
As you will see in the complete document, the residency programs that pay the most are church sponsored hospitals in the northeast. Those that pay the least are state hospitals in the south.








 My name is Andrew and I am a first year resident training to be an ophthalmologist. I created ShortWhiteCoats to provide medical students, residents, and the public with all the information I spent so many hours looking for during medical school.
My name is Andrew and I am a first year resident training to be an ophthalmologist. I created ShortWhiteCoats to provide medical students, residents, and the public with all the information I spent so many hours looking for during medical school.







