An Emergency Medicine Attending Physician's Perspective:
From an interview with an Emergency Medicine physician in Colorado. Part of an interview series entitled, "Specialty Spotlights", which asks medical students' most burning questions to physicians of every specialty. See what doctors from every specialty had to say about why they chose their specialty and how to match in their residency.
How competitive is the Emergency Medicine match?
Emergency Medicine has increased in competitiveness over the last 5-7 years, and seems to fluctuate somewhat in competitiveness. I personally think that competitiveness will maintain or increase as graduates are more attracted to specialties that compensate well while maintaining a good lifestyle (with minimal call), but that remains to be seen.
What must a student do to match into a great Emergency Medicine residency?
As with all specialties in the match, a good score on Step 1 is a must, but additionally a good Step 2 score is also important. EM program directors value this clinical-based test and your ability to perform in a clinical environment. Some say that this score is even more important than Step 1.
More important than either of those is your performance on clinical rotations, shelf exams, and letters of recommendation. Emergency Physicians greatly value working with partners and colleagues who push themselves to be not only be great physicians, but team players who give the effort to help their fellow physicians. You have to go above and beyond with a solid knowledge base, evidence-based practice, and great interpersonal skills.
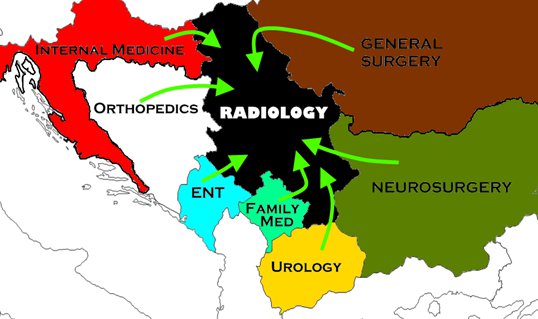
The core 3rd year rotations are especially important (in addition to a sub-internship in EM) as our scope of practice really does encompass a significant portion of every other specialty.
What are residencies looking for in an Emergency Medicine applicant?
What should students look for in an Emergency Medicine residency?
This will vary; you have to prioritize what is most important to you. Important considerations include location, reputation, research and leadership capability / opportunities, faculty, etc. Compensation is a consideration, but I think you (like me) will find that the variability is slight. Some programs offer coverage of meals while working, and some offer full health insurance benefits including dependents. You will find a litany of differences – some of which may be deal breakers, some of which will only be perks – it's up to you to decide what's important.
Most programs have some subtle differences in their rotation schedule, which may make or break the decision for some, but I find that the differences are small, and many programs will provide excellent training. There are some programs which rise above the others for one reason or the other, but these reasons may be different for each applicant. I found that focusing on subtle schedule differences created frustration, and got away from the more important consideration, which was fit.
In my opinion, the most important consideration is how you feel you fit with the program. Does your personality mesh well with your fellow residents and those of the faculty? If you have a family, will they be welcomed at events, or is every out-of-work gathering going to be held at a bar? What is your overall impression of the program, and how does that fit with your goals?
Do you have any advice on the application, letters of recommendation, personal statements, or how to rank programs?
With regards to ranking programs, most of that in my opinion is answered above. It's important to make a list of priorities and stick to it. As for the application, LORs, and personal statement: LORs should be obtained from practicing Emergency Physicians who know you and can speak to your clinical skills as well as personal attributes. Having an impersonal letter from a "big name" in Emergency Medicine is not nearly as important as one from someone who can write a strong letter touting your abilities as a provider as well as a person.
Your personal statement should be concise (no more than a page) and clearly demonstrate WHY you are going to be a rock star EP. However, you should not explicitly write all that out. Find a case that will grab the attention of the reader, demonstrates why you think EM is a no-brainer choice and why you are committed to it, and also showcasing your talents and skills. This is your chance to express how you stand out from your peers, so you need to do that without sounding egotistical. This is not a time for straight humility, but you must represent yourself with quiet confidence.
What do you wish you knew before application/interview season?
Be familiar with the results of the match from recent years, and discuss with your faculty mentors how many programs you need to apply to / interview with. Currently, 9-12 interviews is likely sufficient for the average applicant, but that may vary in coming years, and depending on the applicant. Interviews can be expensive, so consider your top picks ahead of time, but don't be afraid to adjust that list as you visit programs and formulate your impressions. You will likely be surprised about which programs stand out, or which will fall in their rank (I know I was…).
What other advice do you have for students applying for Emergency Medicine residency?
This is a great specialty and profession. While we tout fun procedures, fast-paced shifts, and a great lifestyle, you should make no mistake and know that we work hard. Very hard. We do work that no one else does, and that many shy away from. We are not experts in every field of medicine, but we are masters of resuscitation, emergent airway management, trauma, and critical care. You will hear some people bash Emergency Medicine for not being "experts" in their specific area of expertise – that's by design! I was never trained to be an OB/GYN, but I am trained to recognize and treat OB and GYN related emergencies, referring those non-emergent cases for outpatient follow-up. This does not give us room to slack and provide substandard care, but rather excellent care of urgent and emergent problems, leaving more obscure and less urgent problems to the specialist. Emergency medicine is awesome, enjoy it!
Editor's Note: Applying for residency or preparing for your interviews? I highly recommend First Aid for the Match
, The Successful Match: 200 Rules to Succeed in the Residency Match
, and The Residency Interview: How To Make the Best Possible Impression
.















 My name is Andrew and I am a first year resident training to be an ophthalmologist. I created ShortWhiteCoats to provide medical students, residents, and the public with all the information I spent so many hours looking for during medical school.
My name is Andrew and I am a first year resident training to be an ophthalmologist. I created ShortWhiteCoats to provide medical students, residents, and the public with all the information I spent so many hours looking for during medical school.







