Few ophthalmology residents today learn the art of color fundus drawing. This used to be a fundamental skill required by all ophthalmologists. With the advent of electronic medical records, wide angle fundus photography, and the never ending push to see more patients, the art has nearly died. However, there are a number of reasons why the art should not be ignored by ophthalmology residents; allow me to try and persuade you.
Why should I still be drawing the retina?
First, you will need to be able to read old medical charts; some of which have only fundus drawings without text descriptions of the retina. No matter what form of ophthalmology you practice, you will need to read and interpret these intricate fundus photography. Second, many retina specialists suggest that taking time to produce a proper fundus drawing is the best way to coerce residents and ophthalmologists into a proper, complete retinal examination. Retina specialists in particular have been known to spend more time on a colored pencil drawing of the retina than on the retinal exam itself. Finally, if you are at all interested in a retina fellowship, there are few better ways to impress your old-school retina faculty than to produce great fundus drawings. So, with that in mind, here is a quick primer.
The Fundus Skeleton
A true retina drawing will contain three concentric circles. The first represents the equator, the second represents the ora serrata, and the third represents the pars plana. There should also be 12 tick marks indicating each clock hour of the retina. (See a great example here).
A Work of Art
Next come the colors. A normal retina should have a red hue and most ophthalmologists will color in the entire first two circles (out to the ora serrata) with a light red color. The image on the left is representative of how to draw most common findings in the retina. Feel free to download and print this image, I have found it very useful. Let's break up the details by color.
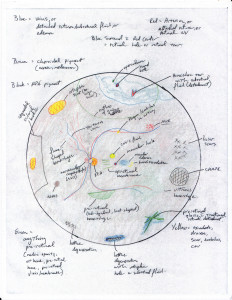
Click for full size [large] image file
Brown:
Click for full size [large] image file
Any alteration in the choroidal pigment. Brown is usually reserved for a nevus or melanoma.
Black:
Any alterations in the retinal pigment including pigment mottling, lattice degeneration, dark retinal pigmentation (CHRPE), or laser scars.
Blue:
A sign of fluid, blue can represent veins, sub retinal fluid surrounding a retinal tear, retinal or macular edema, or a frank retinal detachment.
Red:
As previously stated, normal retina is red and most ophthalmologist paint the entire fundus with a light red color. Arteries are also red and any retinal neovascularization is red as well. A darker red is used inside of a blue outline to demonstrate retinal holes or tears.
Green:
Anything in the pre-retinal space. This includes media opacities, vitreous hemorrhage, pre-retinal hemorrhage, pre-retinal gliosis, epi-retinal membrane.
Yellow:
Exudative processes including retinal exudation, drusen, retinal scars, emboli, choroidal neovascular membranes.
Good Luck!






 My name is Andrew and I am a first year resident training to be an ophthalmologist. I created ShortWhiteCoats to provide medical students, residents, and the public with all the information I spent so many hours looking for during medical school.
My name is Andrew and I am a first year resident training to be an ophthalmologist. I created ShortWhiteCoats to provide medical students, residents, and the public with all the information I spent so many hours looking for during medical school.








